Review Articles
Opioids have no role in patients awaiting total knee arthroplasty
ABSTRACT: End-stage osteoarthritis of the knee can be a debilitating condition that greatly reduces patients’ quality of life. Total knee arthroplasty is an elective operation that can relieve pain and improve functioning but can be inaccessible due to prolonged wait times in British Columbia. An increasing number of patients awaiting total knee arthroplasty have been prescribed opioids to manage their pain in the interim. We review the current literature on opioid use in chronic noncancer pain, with knee osteoarthritis, and prior to total knee arthroplasty; highlight concerns about the practice; and advise against opioid use in this patient population. Given the limited efficacy of opioids relative to other first-line osteoarthritis treatments, adverse effects, worsened postoperative outcomes, uncertain but avoidable risk of substance use disorder, and availability of promising alternative treatments, we recommend against the use of opioids in patients awaiting total knee arthroplasty.
Given their limited efficacy relative to other first-line osteoarthritis treatments, adverse effects, worsened postoperative outcomes, and the uncertain but avoidable risk of substance use disorder, opioids should not be prescribed to patients awaiting total knee arthroplasty.
Total knee arthroplasty is a surgical procedure performed to relieve pain secondary to osteoarthritis of the knee. It is considered in patients who have chronic pain that is severe enough to hinder daily functioning and in cases where first-line pharmacologic and nonpharmacologic arthritis treatments are ineffective.
The procedure can lead to significant improvements in pain, functioning, and quality of life. However, wait times are a barrier for many patients. The BC Surgical Patient Registry estimates that as of 31 March 2022, 8315 patients were awaiting total knee arthroplasty; 90% of surgeries performed between 1 January 2022 and 21 March 2022 had a wait time of 51.4 weeks.[1] These reports may underrepresent the crisis because they do not account for eligible patients who were unable to book or reserve a position on surgical wait lists. This prolonged preoperative period has a serious impact on the quality of life of patients with severe knee osteoarthritis; many self-report on the EuroQoL five-dimension questionnaire as being in a health state “worse than death.”[2]
The wait times for elective procedures have increased since the start of the COVID-19 pandemic, as hospitals shifted toward prioritizing acute care. More than 6 million elective orthopaedic procedures were canceled globally during the first peak of the pandemic.[3]
An increasing number of patients awaiting total knee arthroplasty are receiving opioids to manage their pain in the interim, and the pandemic has bolstered this trend. In the United Kingdom, the median wait times for hip and knee arthroplasty increased from 365 days to 455 days following the outbreak of COVID, and the proportion of patients on any opioid by the time they reached surgical follow-up during that period increased from 41.2% to 55.0%.[4] In Alberta between 2013 and 2015, an estimated 31% of knee osteoarthritis patients were prescribed at least one opioid prior to total knee arthroplasty.[5] While there are no direct data for British Columbia, the prescription of tramadol/tapentadol in surgical specialties increased by 12% between 2013 and 2018.[6] Globally, there has been an overall rapid increase in the use of opioids to manage chronic noncancer pain.[7]
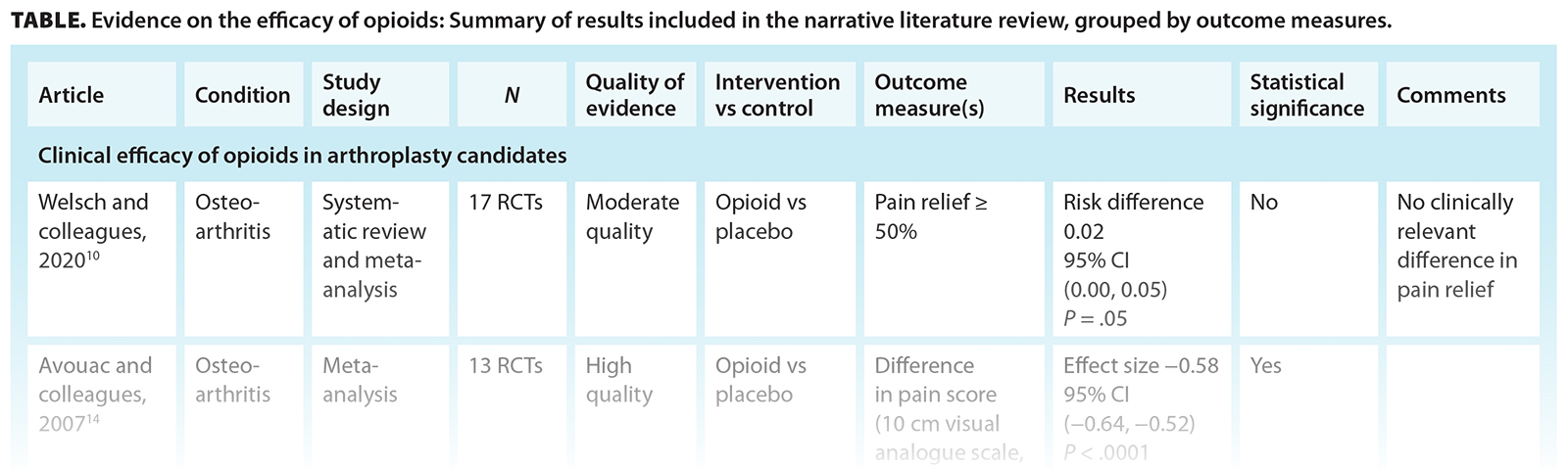
We aim to raise awareness about the growing trend in opioid prescribing in patients awaiting total knee arthroplasty by outlining the current evidence on the efficacy of opioids [Table], their impact on surgical outcomes, and the risk of opioid use disorder in this patient population. We also discuss potential alternative treatments to manage pain prior to total knee arthroplasty.
Clinical efficacy of opioids in arthroplasty candidates
Opioid therapy has been broadly shown to have modest effects in chronic noncancer pain. A recent systematic review examined 42 high-quality randomized controlled trials that followed chronic noncancer pain patients for 3 months or longer. It compared pain reduction between patients prescribed opioids and those on a placebo. While a clinically significant difference was seen in the opioids group, the effect size decreased in studies that followed up with patients for longer periods.[8] The review also examined 51 high-quality randomized controlled trials that compared physical functioning in chronic noncancer pain patients on opioids versus those on placebo and found no clinically significant difference on the 36-item short-form physical component score.[8]
Similar results have been observed in patients with hip and knee osteoarthritis: systematic reviews have demonstrated a decreasing effect on pain relief[9] or no clinically relevant difference in pain relief[10] when opioids were used for more than 1 month. A narrative review of 35 studies on patients with knee osteoarthritis found no clinical difference in patient-reported pain outcomes between opioid and nonopioid users when the drug was used as a long-term therapy.[7]
Some evidence suggests that opioid therapy is not superior to nonopioid first-line medications used by osteoarthritis patients, such as acetaminophen and NSAIDs. Only a limited number of head-to-head trials have compared these analgesics in chronic noncancer pain patients, which has prevented meta-analyses on the topic. However, a recent randomized controlled trial examined the efficacy of different analgesics in chronic hip, back, and knee pain. It compared patients on opioids with those on acetaminophen and NSAIDs and found no significant difference in pain-related function at 12-month follow-up.[11]
The unwanted side effects of opioids must also be considered when evaluating their clinical use. Many patients with chronic noncancer pain tend to discontinue opioid use due to adverse events or insufficient pain management.[12] A recent systematic review on patient preferences in treating chronic noncancer pain found that the adverse effects of opioids may reduce or eliminate any benefit unless pain relief is significant.[13] A meta-analysis of 18 high-quality studies on patients with osteoarthritis found the number needed to harm was 4 for strong opioids and 9 for weak opioids.[14] Another systematic review found that among patients with osteoarthritis in the hip or knee, those on opioids had a pooled risk ratio of 1.49 for any adverse event and a pooled risk ratio of 3.76 of dropping out due to any adverse event, compared with controls.[9]
Effect of opioids on postsurgical outcomes
Presurgical use of opioids has been associated with worse outcomes in both pain and functioning after total knee arthroplasty has been completed. A narrative review of 35 studies found that patients on opioids had a statistically significantly lower Knee Society Score following total knee arthroplasty, had longer in-hospital stays, and had a higher prevalence of subsequent referrals to pain management.[7] A prospective cohort study of 156 patients reported that patients with preoperative opioid use had a smaller improvement in their Western Ontario and McMaster Universities Arthritis Index (WOMAC) pain scores 6 months following total knee arthroplasty than those who were opioid-naive.[15] This disparity continued to be seen 12 months after total knee arthroplasty, with patients on opioids prior to surgery having lower adjusted WOMAC scores and physical functioning scores.[5]
Postoperative pain is one of the most significant factors that determines whether a revision operation is performed.[16] A systematic review found conflicting evidence as to whether preoperative opioid use independently increased the prevalence of revision surgery after joint arthroplasty; one article found an increased rate and three found no difference relative to opioid-naive patients, though all studies were graded as low quality.[17]
Substance use disorder and related outcomes
Evidence suggests there is an increased risk of substance use disorder in patients who are prescribed opioids for chronic pain, but effect sizes are variable. A systematic review of 19 articles, 13 of which presented a low risk of bias, found that problematic opioid use was prevalent in 36.3% of patients with chronic noncancer pain.[18] A second systematic review examined 13 high-quality studies on misuse and 10 high-quality studies on addiction in patients with chronic noncancer pain who were prescribed opioids. The rates of misuse varied from 2.0% to 56.3%, and the rates of addiction ranged from 0.7% to 23.0%.[19]
In the context of osteoarthritis of the knee or hip, moderate-quality evidence from three articles in a larger systematic review indicated that withdrawal symptoms were 1.5% more frequent in patients prescribed opioids compared with those given placebo.[9]
Several articles have examined the risk of prolonged postoperative opioid use following total joint arthroplasty. A recent systematic review of 29 high-quality studies and 1 moderate-quality study found that patients who underwent total knee arthroplasty had rates of postoperative opioid use as follows: at 3 months, 26% (95% CI, 19% to 33%); at 6 months, 20% (95% CI, 17% to 24%); at 9 months, 23% (95% CI, 17% to 28%); and at 12 months, 21% (95% CI, 12% to 29%). It also found that opioid-naive patients were less likely to have continued postoperative opioid use than those who were opioid-tolerant preoperatively.[20]
Discussion
Certain factors, separate from preoperative opioid use, have been found to increase the risk of prolonged opioid use after total knee arthroplasty. They include anxiety, substance misuse, and alcohol misuse.[21] Physicians have commonly used screening tools to gauge a patient’s risk for opioid use disorder before issuing an opioid prescription. However, a recent review article noted that the two most commonly used risk assessment tools in BC—the Opioid Risk Tool and the Prescription Opioid Misuse Index—are based on lower-quality studies and have poor predictive accuracy.[22] Given the uncertainty of prognosis even after screening, avoiding prescribing opioids to patients who are awaiting total knee arthroplasty, especially considering opioids’ lack of efficacy, may be the safest option.
There is clinical equipoise on whether long-acting versus short-acting opioids lead to better outcomes in patients with chronic noncancer pain. However, a qualitative systematic review of six randomized trials found no difference in pain relief, consumption of rescue analgesia, quality of sleep, or physical functioning. It noted that these findings challenge several guidelines that recommend long-acting opioids as a safer option.[23] In the experience of the senior authors, the use of long-acting opioids is much more difficult to taper off, which results in a higher rate of dependence; therefore, their use needs to be avoided in patients with chronic noncancer pain.
Many current guidelines caution against the use of opioids in patients with knee osteoarthritis and in those awaiting total knee arthroplasty. The American College of Rheumatology and the Arthritis Foundation recommend using tramadol for knee osteoarthritis only if the patient has contraindications to NSAIDs, has no available surgical options, and finds other therapies ineffective. It also advises against prescribing nontramadol opioids in this patient group unless alternative treatments have been exhausted, and even then, the lowest possible dose for the shortest possible length is recommended.[24] Guidelines from the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases recommend the use of opioids only as a last step before osteoarthritis surgery; the slow titration of sustained-release tramadol, a weak opioid, affords sustained analgesia with improved tolerability.[25] A recent review article of United States data recommended that during the perioperative period for total joint arthroplasty, opioids be prescribed only when absolutely necessary, at their lowest dose, and for the shortest duration necessary to control symptoms; close monitoring of common adverse effects should also be conducted.[26]
Novel minimally invasive procedures
Minimally invasive procedures have shown promise as alternative pain management options in patients awaiting total knee arthroplasty. Specifically, genicular artery embolization has demonstrated safety, good efficacy, and no serious complications in multiple preliminary clinical trials.[27] Further investigation into techniques such as genicular artery embolization may lead to breakthroughs in patient care and revision of current management algorithms. To this effect, the World Health Organization has added minimally invasive procedures as a step on its analgesic ladder.[28]
Pain as a psychosocial issue
Pain is a complex psychosocial issue, and an individual’s response to a given level of nociception can vary based on their circumstances, mental health, mindset, and coping mechanisms.[16] Some factors associated with preoperative opioid use in knee osteoarthritis include comorbid spine osteoarthritis, higher symptomatic joint count, depressive symptoms, obesity, being a current or former smoker, and current use of other prescription pain medication,[29] all of which may be linked to social determinants of health.
While avoiding opioids is ideal for opioid-naive patients awaiting total knee arthroplasty, many individuals undergoing joint replacement in Canada and the United States are already on potent opioids.[16] It is especially important in these patients to use a harm reduction approach and provide psychosocial support. There is preliminary evidence that brief psychological interventions may reduce prescription opioid–related harm in patients with chronic pain.[30]
Summary
End-stage osteoarthritis of the knee can be a debilitating condition that greatly lowers patients’ quality of life. Total knee arthroplasty is an elective operation that can relieve pain and improve functioning, but it can be inaccessible due to prolonged wait times in BC. An increasing number of patients awaiting total knee arthroplasty have been prescribed opioids to manage their pain in the interim. Given the limited efficacy of opioids relative to other first-line osteoarthritis treatments, adverse effects, worsened postoperative outcomes, uncertain but avoidable risk of substance use disorder, and the presence of promising alternative treatments, we recommend against their use in patients awaiting total knee arthroplasty. Novel minimally invasive procedures such as genicular artery embolization may help reduce the need for presurgical opioid use. From a systems perspective, sustained efforts at shortening wait times for consultation with orthopaedic surgeons and improving access to surgical services would obviate the need to prescribe opioids and diminish the iatrogenic contribution to the opioid crisis in BC.
Competing interests
None declared.
This article has been peer reviewed.
 |
| This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. |
References
1. British Columbia Ministry of Health. Surgery wait times for “adult—knee replacement.” Surgery wait times. Accessed 23 April 2022. https://swt.hlth.gov.bc.ca/swt/WaitTimesResults.xhtml?rollupProcedure=58&procName=Knee+Replacement&adult=Y.
2. Clement ND, Scott CEH, Murray JRD, et al. The number of patients “worse than death” while waiting for a hip or knee arthroplasty has nearly doubled during the COVID-19 pandemic. Bone Joint J 2021;103-B:672-680.
3. COVIDSurg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: Global predictive modelling to inform surgical recovery plans. Br J Surg 2020;107:1440-1449.
4. Farrow L, Gardner WT, Tang CC, et al. Impact of COVID-19 on opioid use in those awaiting hip and knee arthroplasty: A retrospective cohort study. BMJ Qual Saf 2023;32:479-484.
5. Goplen CM, Kang SH, Randell JR, et al. Effect of preoperative long-term opioid therapy on patient outcomes after total knee arthroplasty: An analysis of multicentre population-based administrative data. Can J Surg J 2021;64:E135-E143.
6. Yefet LS, Bone JN, Courtemanche R, et al. Opioid prescribing patterns in British Columbia from 2013 to 2017: A population-based study. BCMJ 2021;63:336-342.
7. Lee B, Sodhi N, Anis HK, et al. Injection alternatives for the management of knee osteoarthritis pain. Surg Technol Int 2019;34:513-519.
8. Busse JW, Wang L, Kamaleldin M, et al. Opioids for chronic noncancer pain: A systematic review and meta-analysis. JAMA 2018;320:2448-2460.
9. da Costa BR, Nüesch E, Kasteler R, et al. Oral or transdermal opioids for osteoarthritis of the knee or hip. Cochrane Database Syst Rev 2014;(9):CD003115.
10. Welsch P, Petzke F, Klose P, Häuser W. Opioids for chronic osteoarthritis pain: An updated systematic review and meta-analysis of efficacy, tolerability and safety in randomized placebo-controlled studies of at least 4 weeks double-blind duration. Eur J Pain 2020;24:685-703.
11. Krebs EE, Gravely A, Nugent S, et al. Effect of opioid vs nonopioid medications on pain-related function in patients with chronic back pain or hip or knee osteoarthritis pain: The SPACE randomized clinical trial. JAMA 2018;319:872-882.
12. Noble M, Treadwell JR, Tregear SJ, et al. Long-term opioid management for chronic noncancer pain. Cochrane Database Syst Rev 2010;(1):CD006605.
13. Goshua A, Craigie S, Guyatt GH, et al. Patient values and preferences regarding opioids for chronic noncancer pain: A systematic review. Pain Med 2018;19:2469-2480.
14. Avouac J, Gossec L, Dougados M. Efficacy and safety of opioids for osteoarthritis: A meta-analysis of randomized controlled trials. Osteoarthritis Cartilage 2007;15:957-965.
15. Smith SR, Bido J, Collins JE, et al. Impact of preoperative opioid use on total knee arthroplasty outcomes. J Bone Joint Surg Am 2017;99:803-808.
16. Agrawal Y, Smith RM, Garbuz DS, Masri BA. Opioids in arthroplasty: Mind the gap between North America and the rest of the world. J Bone Joint Surg Am 2018;100:2162-2171.
17. Hannon CP, Fillingham YA, Nam D, et al. The efficacy and safety of opioids in total joint arthroplasty: Systematic review and direct meta-analysis. J Arthroplasty 2020;35:2759-2771.e13.
18. Jantarada C, Silva C, Guimarães-Pereira L. Prevalence of problematic use of opioids in patients with chronic noncancer pain: A systematic review with meta-analysis. Pain Pract 2021;21:715-729.
19. Vowles KE, McEntee ML, Julnes PS, et al. Rates of opioid misuse, abuse, and addiction in chronic pain: A systematic review and data synthesis. Pain 2015;156:569-576.
20. Tay HP, Wang X, Narayan SW, et al. Persistent postoperative opioid use after total hip or knee arthroplasty: A systematic review and meta-analysis. Am J Health Syst Pharm 2022;79:147-164.
21. Schwenk ES, Pozek J-PJ, Viscusi ER. Managing prolonged pain after surgery: Examining the role of opioids. J Arthroplasty 2018;33:3389-3393.
22. Klimas J, McCracken RK, Bassett K, Wood E. Think twice: Evidence-based opioid sparing approaches to pain management. BCMJ 2020;62:234-237.
23. Pedersen L, Borchgrevink PC, Riphagen II, Fredheim OMS. Long- or short-acting opioids for chronic non-malignant pain? A qualitative systematic review. Acta Anaesthesiol Scand 2014;58:390-401.
24. Kolasinski SL, Neogi T, Hochberg MC, et al. 2019 American College of Rheumatology/Arthritis Foundation guideline for the management of osteoarthritis of the hand, hip, and knee. Arthritis Care Res 2020;72:149-162.
25. Bruyère O, Cooper C, Pelletier JP, et al. A consensus statement on the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) algorithm for the management of knee osteoarthritis—From evidence-based medicine to the real-life setting. Semin Arthritis Rheum 2016;45(Suppl):S3-S11.
26. Lespasio MJ, Guarino AJ, Sodhi N, Mont MA. Pain management associated with total joint arthroplasty: A primer. Perm J 2019;23:18-169.
27. Torkian P, Golzarian J, Chalian M, et al. Osteoarthritis-related knee pain treated with genicular artery embolization: A systematic review and meta-analysis. Orthop J Sports Med 2021;9:23259671211021356.
28. Anekar AA, Hendrix JM, Cascella M. WHO analgesic ladder. In: StatPearls. Treasure Island, FL: StatPearls Publishing, 2021. Accessed 22 September 2021. www.ncbi.nlm.nih.gov/books/NBK554435.
29. Power JD, Perruccio AV, Gandhi R, et al. Factors associated with opioid use in presurgical knee, hip, and spine osteoarthritis patients. Arthritis Care Res 2019;71:1178-1185.
30. Elphinston RA, Sterling M, Leung J, et al. Brief psychological interventions for reducing prescription opioid use, related harm, and pain intensity in patients with chronic pain: A systematic review and assessment of patient interest. Clin J Pain 2021;37:270-280.
Mr Marcuzzi is a medical student at the University of British Columbia. Dr Liu is an interventional radiologist at Vancouver General Hospital and UBC Hospital and an associate professor at the UBC School of Biomedical Engineering. Dr Badii is a clinical assistant professor in the Division of Rheumatology, Faculty of Medicine, UBC. Dr Masri is a professor of orthopaedics at UBC and an orthopaedic surgeon at Vancouver General Hospital and UBC Hospital.